Biliopancreatic Diversion
Introduction
Biliopancreatic diversion surgery changes the normal process of digestion by making the stomach smaller, allowing the food to bypass a part of the small intestine so that fewer calories are absorbed. Because of some associated risks, this surgery is only performed on people who are severely obese and who have failed to lose weight by any other means. Severe obesity means that the BMI (Body Mass Index) is 50 or higher.
After the operation the patient feels full more quickly than when the stomach was its original size, this subsequently reduces the amount of food eaten. Bypassing part of the intestine also means that fewer calories are absorbed.
The procedure
There are two types of these procedures:
1. Biliopancreatic diversion
2. Biliopancreatic diversion with duodenal switch
We have all the information you need about public and private clinics and hospitals that provide weight loss surgeries in Iran, Islamic Republic Of with the best quality and lowest possible prices
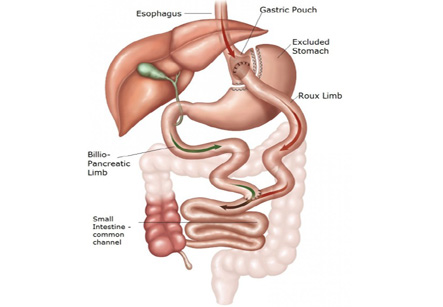
Most bariatric surgeons will not perform duodenal switch surgery unless the person is severely obese (BMI of 50 or higher) and the weight is causing serious health problems. In a biliopancreatic diversion, a part of the stomach is removed, then the remaining part of the stomach is connected to the lower portion of the small intestine. This type of bariatric surgery is considered a high-risk procedure with some potential for long-term health problems, as the body could struggle to absorb food and nutrients.
Most people lose 75% to 80% of their excess weight and able to stay at their new weight.
In a biliopancreatic diversion with duodenal switch, a different part of the stomach is removed saving the pylorus which is the valve controlling food drainage from the stomach. This is also a high-risk surgery. After both of these surgeries, vitamin and mineral supplements need to be taken for the rest of the patient’s life, which can in turn become quite expensive.
These procedures can be done by making a large incision in the abdomen (an open procedure) or by making small cuts and using small tools and a camera to guide the surgery (laparoscopy).
Considerations after surgery
Some abdominal pain is normal after surgery and the patient may need pain medicine aid for the first week or so after surgery. The chosen obesity doctor will provide the patient with specific instructions on what to eat (and what to avoid) after surgery. For about the first month after the operation, the stomach can only handle small amounts of soft foods and liquids and so it is important to sip water throughout the day to avoid becoming dehydrated. The bowel movements may not be regular after the surgery, constipation and straining with bowel movements should be avoided.
Gradually, solid foods are added back into the diet. Be careful to chew food well and stop eating when you feel full, although it sounds easy to do it can take some time getting used to. If the food is not chewed well or if the patient does not stop eating soon enough, some discomfort or nausea and vomiting may occur. If high calorie liquids such as soda or fruit juice are taken, there may be no loss of weight and the same occurs if over-eating is continued, the stomach may stretch and the benefit from surgery is void.
Depending on how the surgery was done (open or laparoscopic) the activity is monitored during recovery. In case of open surgery, heavy lifting or strenuous exercise should be avoided while recovering, and the patient may be able to return to work or to a normal routine in 4 to 6 weeks.
General indications
Weight loss surgery is suitable for people who are severely overweight and who have not been able to lose weight with a diet, exercise, or medicine. Surgery is generally considered when:
1. The body mass index (BMI) is 40 or higher
2. BMI is 35 or higher, associated with a life-threatening problem that is related to body weight
However, the surgery is not an instant fix, the patient will still need to eat a healthy diet and get regular exercise. This will help to reach the weight goal and avoid regaining the weight after treatment.
Typical results
Biliopancreatic diversion surgery is effective as most people lose 75% to 80% of their excess weight and are able to stay at their new weight, though many patients seek excess skin surgery at some point after treatment. The long-term success is highest in people who are realistic about the goal of weight loss, keep regular follow-up with the medical team, follow the eating plan made by the dietician or nutritionist, and are physically active.
Risks to be considered
Risks commonly associated to all types of weight loss surgery include:
1. Infection in the incision
2. A leak from the stomach into the abdominal cavity
3. A leak at the intestinal connection
4. Blood clots in the legs which may travel to lungs
5. Gallstones
Biliopancreatic diversion surgery may offer short and long-term risks such as:
1. Dumping syndrome causes nausea, weakness, sweating, faintness, and possibly diarrhea soon after eating due to early stomach emptying. These symptoms get worse due to eating highly refined, high-calorie foods (like sweets)
2. A higher risk of osteoporosis and anemia as the body cannot absorb nutrients properly
3. Bad smelling stools and diarrhea. This occurs because of poor absorption of protein, fat, calcium, iron, and vitamins B12, A, D, E, and K.
4. Poor nutrition. Eating less and less absorption can cause health problems due to lack of nutrients